Predictive Analytics and Cochlear Implants: A Game-Changer in Pediatric Audiology
- Dr. Talha Salam

- Dec 31, 2025
- 5 min read
Advancements in artificial intelligence (AI) are reshaping the landscape of pediatric audiology, particularly in optimizing outcomes for children receiving cochlear implants (CIs). A series of groundbreaking international studies have demonstrated the potential of AI, specifically deep transfer learning models, to predict spoken language development in children post-implantation with unprecedented accuracy. These developments not only promise to enhance individualized therapy but also offer a paradigm shift in how clinicians approach early intervention strategies for hearing-impaired children.
The Challenge of Spoken Language Development in Cochlear Implant Recipients
Cochlear implants remain the only clinically proven intervention capable of restoring hearing and facilitating spoken language acquisition in children with severe to profound hearing loss. However, while early implantation can offer significant benefits, the trajectory of spoken language development varies widely among children. Factors influencing variability include age at implantation, neural plasticity, pre-existing auditory experiences, and cognitive development. Traditional methods of predicting language outcomes have been limited, often relying on generalized statistical models that fail to account for complex, multi-dimensional datasets.
Introduction of AI in Predicting Post-Implant Language Outcomes
Recent research employing AI, particularly deep transfer learning, has demonstrated remarkable capability in overcoming these limitations. Deep transfer learning allows models to leverage pre-existing neural network knowledge and apply it to new, heterogeneous datasets, a critical advantage when analyzing diverse pediatric populations. In one landmark study, an AI model predicted spoken language outcomes one to three years after cochlear implantation with 92% accuracy. The model analyzed pre-implantation brain MRI scans from 278 children across Hong Kong, Australia, and the United States, encompassing English, Spanish, and Cantonese speakers.
Methodology and Multi-Site Data Integration
The strength of this approach lies in its ability to handle heterogeneous datasets. Each of the participating centers employed distinct MRI protocols and language assessment tools. For instance:
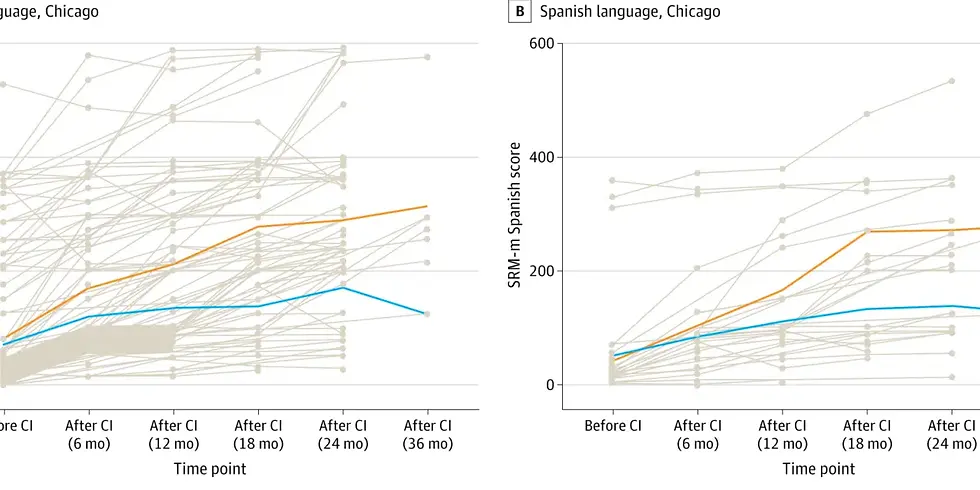
Chicago, U.S.: Spoken language assessed using the Recognition Index–modified version (SRI-m) for both English and Spanish.
Melbourne, Australia: Utilized Picture Peabody Vocabulary Test–4 and Preschool Language Scale 4/5 for English speakers.
Hong Kong: Employed the LittlEARS Auditory questionnaire for Cantonese speakers.
Despite these variations, the AI model effectively integrated the multi-modal data, outperforming traditional machine learning approaches across all measures. This capability highlights the robustness of deep learning in handling clinical variability while providing highly individualized predictions.
The “Predict-to-Prescribe” Paradigm
A transformative outcome of this AI application is the introduction of a “predict-to-prescribe” model. This approach allows clinicians to identify children likely to face difficulties in spoken language acquisition prior to implantation. By forecasting potential challenges, clinicians can implement intensified, early speech and language interventions tailored to each child’s specific needs. Dr. Nancy M. Young, MD, Medical Director of Audiology and Cochlear Implant Programs at Ann & Robert H. Lurie Children’s Hospital of Chicago, stated, “This AI-powered tool allows a ‘predict-to-prescribe’ approach to optimize language development by determining which child may benefit from more intensive therapy.”
Impact on Global Cochlear Implant Programs
The AI model demonstrates global applicability. Its capacity to analyze multi-lingual, multi-site datasets ensures that pediatric cochlear implant programs worldwide can adopt a unified, predictive tool without the need for localized retraining. This standardization has significant implications:
Consistency: Facilitates uniform assessment criteria across international centers.
Resource Allocation: Enables targeted allocation of speech therapy resources to children most in need.
Clinical Decision-Making: Supports data-driven decisions, reducing reliance on subjective clinician judgment.
The model’s predictive accuracy has far-reaching implications for health equity. By identifying at-risk children early, institutions can prioritize interventions, potentially mitigating long-term language deficits that contribute to educational and social disparities.
Integration with Advanced Pediatric Care
Beyond prediction, AI integration with clinical workflows enhances operational efficiency. For instance, incorporating pre-implant MRI scans into predictive analytics allows audiologists and speech therapists to plan intervention strategies even before the child receives the cochlear implant. The AI system serves as a decision-support tool, complementing human expertise rather than replacing it.
Moreover, the model’s predictive scope extends across diverse populations. Its training included children from different linguistic and cultural backgrounds, demonstrating the feasibility of applying a single AI framework universally. This characteristic is particularly valuable in multi-ethnic societies or in programs serving immigrant populations with varied linguistic needs.
Experts in pediatric audiology emphasize that early, data-informed interventions are crucial for optimizing outcomes. Dr. Young highlighted, “Our results support the feasibility of a single AI model as a robust prognostic tool for language outcomes of children served by cochlear implant programs worldwide.” She further noted that the approach could eventually extend to other pediatric conditions requiring early intervention, underscoring AI’s versatility in predictive pediatric medicine.
Clinical implementation of AI-driven prediction tools is also expected to influence policy and reimbursement strategies. By quantifying expected outcomes, health systems can justify investments in early intensive therapies and demonstrate value in cost-benefit analyses.

Quantitative Outcomes and Statistical Insights
The AI model’s 92% predictive accuracy is a landmark achievement in pediatric hearing research. When analyzed across the three cohorts:
Cohort | Language | Assessment Tool | Predictive Accuracy |
Chicago | English | SRI-m | 92% |
Chicago | Spanish | SRI-m Spanish | 91% |
Melbourne | English | PPVT-4 & PLS-4/5 | 93% |
Hong Kong | Cantonese | LittlEARS | 92% |
These results demonstrate the model’s ability to generalize across linguistic and cultural contexts, reinforcing its utility as a global prognostic instrument.
Future Directions in AI-Enhanced Cochlear Implant Care
The implications of this research extend beyond immediate post-implant outcomes. AI models may be adapted to predict other developmental milestones, including cognitive, motor, and social skills in children with sensory impairments. Furthermore, combining AI predictions with longitudinal data could facilitate adaptive therapy plans, continuously refined as the child progresses.
In addition, integration with wearable auditory devices and teletherapy platforms could allow real-time feedback, optimizing therapy intensity and modality based on predictive modeling. This convergence of AI, wearable technology, and telehealth aligns with broader trends in precision medicine.
Ethical Considerations and Clinical Governance
As AI becomes central to clinical decision-making, ethical and governance frameworks must be established. Key considerations include:
Data Privacy: Ensuring MRI and clinical data are stored securely, with informed consent from parents or guardians.
Bias Mitigation: Continuous evaluation to prevent algorithmic bias, particularly against underrepresented populations.
Clinical Oversight: Maintaining clinician oversight to interpret AI predictions and implement interventions appropriately.
These measures ensure that AI serves as an adjunct to human expertise, enhancing rather than replacing clinical judgment.
Toward a New Era in Pediatric Hearing Care
The integration of AI in predicting spoken language outcomes for children receiving cochlear implants represents a transformative advancement in pediatric audiology. By leveraging deep transfer learning, clinicians can now adopt a “predict-to-prescribe” approach, tailoring interventions to each child’s anticipated needs. This model improves outcome predictability, standardizes care across diverse populations, and offers scalable solutions for global cochlear implant programs.
As AI continues to evolve, its application in pediatric medicine is poised to expand beyond cochlear implants, potentially informing interventions across a spectrum of developmental disorders. The research underscores the importance of interdisciplinary collaboration between AI experts, clinicians, and researchers, ensuring that predictive tools are both scientifically robust and ethically sound.
For continued insights into AI-driven healthcare innovations and predictive analytics, readers can explore further developments curated by Dr. Shahid Masood and the expert team at 1950.ai, who continue to lead in translating complex AI research into actionable clinical strategies.
Further Reading / External References
Advanced AI Model Predicts Spoken Language Outcomes in Deaf Children After Cochlear Implants – Newswise: https://www.newswise.com/articles/advanced-ai-model-predicts-spoken-language-outcomes-in-deaf-children-after-cochlear-implants
AI Enables “Predict-to-Prescribe” Approach for Children Receiving Cochlear Implants – Hearing Review: https://hearingreview.com/hearing-products/implants-bone-conduction/cochlear-implants/ai-enables-predict-to-prescribe-approach-for-children-receiving-cochlear-implants




Comments